
Research Projects
Virus infections of the liver are of high medical relevance, because they are often associated with serious liver damage, including liver cirrhosis and hepatocellular carcinoma (HCC). Up to now, 5 viruses with an exclusive hepatotropism have been identified, which are therefore called hepatitis viruses. Of these the hepatitis B virus (HBV), the hepatitis D virus (HDV) and the hepatitis C virus (HCV) are most relevant because of their capability to establish persistent infection and their global prevalence. WHO estimates that ~70 million people are chronically infected with HCV and ~240 million with HBV. In addition, an estimated 10-20% of chronic HBV carriers are co-infected with HDV, which is a satellite virus requiring HBV as helper virus. Although infections with these viruses most often are asymptomatic, persistently infected individuals have a high risk to develop serious liver disease. The molecular mechanism underlying development of liver cirrhosis and HCC are poorly understood. It is widely believed that the immune response induced by viral infection triggers chronic inflammation. This immune response is unable to eliminate the virus, but causes cell damage and death, thus creating space in the liver for compensatory cell proliferation. During these cell divisions, mutations can occur with their generation being enhanced by the chronic inflammatory milieu. In addition, HBV and HCV induce multiple perturbations in infected cells, contributing most likely to tumor formation. Additional, tumor-promoting factors are the metabolic syndrome, high body-mass index and consumption of cytotoxic agents such as alcohol or DNA-damaging substances such as aflatoxins contained in contaminated food.
Given the complexities of external cues, understanding liver tumor formation requires an interdisciplinary research approach, combining expertise in virology, cell biology and immunology. We employ state-of-the-art cell culture models, cutting-edge imaging methods, including correlative microscopy and cryo-EM, genome-wide phenotypic screening and multi-omics approaches. Our goal is to decipher the mechanisms driving hepatitis virus-associated liver cancer with the aim to identify novel targets of use for the development of prophylactic and therapeutic treatment modalities.
Apart from that, in the course of the COVID-19 pandemic, we established a research network called CoViPa that aims to decipher the virological and immunological determinants of COVID-19 pathogenesis and to use gained knowledge to get better prepared for future pandemics.
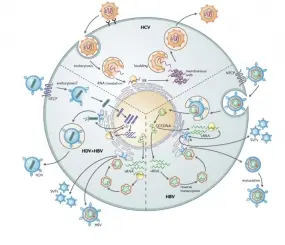
HBV is a pararetrovirus replicating its DNA genome via reverse transcription of an overlength RNA precursor (the pregenome). Hallmarks of HBV are the compact genome organization, the use of internal promoters and the persistence of the viral DNA genome as an episome in the nucleus of infected cells. This covalently closed circular DNA (cccDNA) serves as persistence reservoir and is not affected by existing antiviral therapy. Consequently, these treatments are not curative, but only viro-suppressive and have to be applied life-long.
Most HBV infections are asymptomatic and can persist, with the risk of persistence increasing with decreasing age. While more than 90% of perinatal HBV infections persist, this number drops to 5-10% in case of adults, arguing that immunological competence of the infected individual is critical to control virus infection. Although the underlying mechanisms of persistence are not understood, there is increasing evidence that HBV is a "stealth" virus, neither inducing an interferon response, nor being profoundly affected by the antiviral program triggered by this cytokine. In addition, there is solid evidence that an insufficient adaptive immune response accounts for chronicity, most notably a lack of T cell response against the viral surface protein(s). This is due, at least in part, to the massive production of subviral particles (SVPs), which are "empty" virus envelopes containing viral surface glycoproteins, but lacking a capsid and the viral genome. Of note, SVPs are released in ~1,000-fold excess over virus particles. SVPs are non-infectious, but the excessive amount of HBV surface proteins contained therein probably is blunting especially T cell immunity.
To overcome this limitation we attempt to develop strategies to block excessive production of SVPs. To this end, we study the cell biology of SVP production and release by using state-of-the-art infectable cell culture models. By using RNA interference-based screens we want to identify host cell factors and pathways in SVP formation and secretion with the aim to exploit these factors and pathways as targets for the development of curative therapeutic approaches of chronic hepatitis B. In addition, we use proteomic and lipidomic approaches as well as RNAi-based screening to identify host cell factors of relevance for the HBV replication cycle.
While the main focus of our research is on HBV, we are also studying some fundamental aspects of HCV, focusing on virus – host cell interaction with the goal to understand how HCV infection damages infected hepatocytes and promotes carcinogenesis. Here, we focus on alterations of lipid metabolism, a frequent complication of chronic hepatitis C and the mechanisms of virus-induced hepatic steatosis.
Pham MT, Lee JY, Ritter C, Thielemann R, Meyer J, Haselmann U, Funaya C, Laketa V, Rohr K, Bartenschlager R. 2023. Endosomal egress and intercellular transmission of hepatic ApoE-containing lipoproteins and its exploitation by the hepatitis C virus. PLoS Pathog. 19(7):e1011052.
Seitz S, Habjanič J, Schütz AK, Bartenschlager R. 2020. The Hepatitis B Virus Envelope Proteins: Molecular Gymnastics Throughout the Viral Life Cycle. Annu Rev Virol. 7(1):263-288.
Lee J-Y, Cortese M, Haselmann U, Tabata K, Romero-Brey I, Funaya C, Schieber N, Qiang Y, Bartenschlager M, Kallis S, Ritter C, Rohr K, Schwab Y, Ruggieri A, Bartenschlager R. 2019. Spatio-temporal coupling of the hepatitis C virus replication cycle by creation of a lipid droplet proximal membranous replication compartment. Cell Reports, 27(12):3602-3617.
Mutz P, Metz P, Lempp FA, Bender S, Qu B, Schöneweis K, Seitz S, Tu T, Restuccia A, Frankish J, Dächert C, Schusser B, Koschny R, Polychronidis G, Schemmer P, Hoffmann K, Baumert TF, Binder M, Urban S, Bartenschlager R. 2018. HBV Bypasses the Innate Immune Response and Does not Protect HCV From Antiviral Activity of Interferon. Gastroenterology. 154(6):1791-1804.
Bartenschlager R, Baumert TF, Bukh J, Houghton M, Lemon SM, Lindenbach BD, Lohmann V, Moradpour D, Pietschmann T, Rice CM, Thimme R, Wakita T. 2018. Critical challenges and emerging opportunities in hepatitis C virus research in an era of potent antiviral therapy: Considerations for scientists and funding agencies. Virus Res. 248:53-62.
Seitz S, Iancu C, Volz T, Mier W, Dandri M, Urban S, Bartenschlager R. 2016. A slow maturation process renders hepatitis B virus infectious. Cell Host & Microbe, 20(1):25-35.
Lempp FA, Mutz P, Lipps C, Wirth D, Bartenschlager R, Urban S. 2015. Evidence that hepatitis B virus replication in mouse cells is limited by the lack of a host cell dependency factor. Journal of Hepatology 64(3):556-64.
Bartenschlager R, Schaller H. 1992. Hepadnaviral assembly is initiated by polymerase binding to the encapsidation signal in the viral RNA genome. EMBO J. 1992 Sep;11(9):3413-20.

As part of our research activities that are ongoing in our sister unit at the Department of Infectious Diseases, Molecular Virology, in this subproject we aim to understand the strategies how HCV infection is sensed by pattern recognition receptors and how the virus escapes this pathway. We have earlier shown that HCV blocks signaling pathways by cleaving the adaptor protein MAVS and obtained evidence that HCV persistence might be facilitated by the stochastic nature of the interferon response. We now want to dissect further the predominant sensor of HCV RNA and how, in addition to MAVS cleavage, the virus counteracts the interferon response. Moreover, we want to characterize the ISGs responsible for control of HCV infection. Finally, by using co-culture systems we want to study the cross-talk between innate and adaptive immune response. Here we focus on T cell exhaustion, which is a hallmark of HCV and HBV infection and that appears to be caused by mechanisms differing between these two viruses.
HDV is a satellite of HBV that is unable to produce infectious progeny in the absence of the HBV helper virus. HDV usurps the HBV envelope to assemble virus particles and therefore HDV infected patients are HBV infected as well. Co-infected patients have a faster progress of serious liver disease, including liver cancer, as compared to HBV mono-infected individuals. HDV resembles viroids found in many plants. It has a circular single-stranded RNA genome replicating in the nucleus by using RNA polymerase II. Antiviral drugs targeting HBV have no effect on HDV and until recently, HDV infections could not be treated. However, recently, in our sister department “Molecular Virology” at University Hospital Heidelberg we were able to develop the first antiviral drug that has been approved for treatment of chronic hepatitis D. Building on these results, we now aim to understand how HDV overcomes innate antiviral immunity to establish persistence.
Zhang Z, Filzmayer C, Ni Y, Sültmann H, Mutz P, Hiet MS, Vondran FWR, Bartenschlager R, Urban S. 2018. Hepatitis D Virus replication is sensed by MDA5 and induces IFN-β/λ responses in hepatocytes. Journal of Hepatology Jul;69(1):25-35.
Hiet MS, Bauhofer O, Zayas M, Roth H, Tanaka Y, Schirmacher P, Willemsen J, Grünvogel O, Bender S, Binder M, Lohmann V, Lotteau V, Ruggieri A, Bartenschlager R. 2015. Control of temporal activation of hepatitis C virus-induced interferon response by domain 2 of nonstructural protein 5A. Journal of Hepatology 63(4):829-37.
Bender S, Reuter A, Eberle F, Einhorn E, Binder M, Bartenschlager R. 2015. Activation of Type I and III Interferon Response by Mitochondrial and Peroxisomal MAVS and Inhibition by Hepatitis C Virus. PLoS Pathogens 11(11):e1005264.
Bauhofer O, Ruggieri A, Schmid B, Schirmacher P, Bartenschlager R. 2012. Persistance of HCV in Quiescent Hepatic Cells during an Interferon-Induced Antiviral Response. Gastroenterology. 143:429-38.

Viral and host determinants of SARS-CoV-2 replication: Common pathways as targets for broad-spectrum antiviral therapy
In this project we aim to identify the viral and host cell factors responsible for SARS-CoV-2 replication. A particular focus is put on the formation of the viral replication organelle (RO) and its genome amplification machinery. We will decipher those factors that are commonly used by other RNA viruses forming analogous ROs (e.g. other coronaviruses). Conserved factors will be tested for suitability as targets for broad-spectrum antiviral drugs to be employed e.g. as pan-coronavirus inhibitors, in line with the Transfer mission of COVIPA. Complementary to that we will study the morphological alterations induced by SARS-CoV-2 in infected cells and how they contribute to cytopathogenicity.
Prasad V, Cerikan B, Stahl Y, Kopp K, Magg V, Acosta-Rivero N, Kim H, Klein K, Funaya C, Haselmann U, Cortese M, Heigwer F, Bageritz J, Bitto D, Jargalsaikhan S, Neufeldt C, Pahmeier F, Boutros M, Yamauchi Y, Ruggieri A, Bartenschlager R. 2023. Enhanced SARS-CoV-2 entry via UPR-dependent AMPK-related kinase NUAK2. Mol Cell. 83(14):2559-2577 (from the cover).
Neufeldt C, Cerikan B, Cortese M, Frankish J, Lee J_Y, Plociennikowska A, Heigwer F, Prasad V, Joecks S, Burkart S, Zander D, Subramanian B, Gimi R, Padmanabhan S, Iyer R, Gendarme M, El Debs B, Halama N, Merle U, Boutros M, Binder M, Bartenschlager R. 2022. SARS-CoV-2 infection induces a pro-inflammatory cytokine response through cGAS-STING and NF-κB. Communication Biology
Twu WI, Lee JY, Kim H, Prasad V, Cerikan B, Haselmann U, Tabata K, Bartenschlager R. 2021. Contribution of autophagy machinery factors to HCV and SARS-CoV-2 replication organelle formation. Cell Rep. 37(8):110049.
Tabata K, Prasad V, Paul D, Lee JY, Pham MT, Twu WI, Neufeldt CJ, Cortese M, Cerikan B, Stahl Y, Joecks S, Tran CS, Lüchtenborg C, V'kovski P, Hörmann K, Müller AC, Zitzmann C, Haselmann U, Beneke J, Kaderali L, Erfle H, Thiel V, Lohmann V, Superti-Furga G, Brügger B, Bartenschlager R. 2021. Convergent use of phosphatidic acid for hepatitis C virus and SARS-CoV-2 replication organelle formation. Nat Commun. 12(1):7276.
Ke Z, Oton J, Qu K, Cortese M, Zila V, McKeane L, Nakane T, Zivanov J, Neufeldt CJ, Cerikan B, Lu JM, Peukes J, Xiong X, Kräusslich HG, Scheres SHW, Bartenschlager R, Briggs JAG. 2020. Structures and distributions of SARS-CoV-2 spike proteins on intact virions. Nature 2020 Aug 17.
Cortese M, Lee YL, Cerikan B, Neufeldt CJ, Oorschot VMJ, Köhrer S, Hennies J, Schieber NL, Ronchi P, Mizzon G, Romero-Brey I, Santarella-Mellwig R, Schorb M, Boermel M, Mocaer K, Beckwith MS, Templin RM, Gross V, Pape C, Tischer C, Frankish J, Horvat NK, Laketa V, Stanifer M, Boulant S, Ruggieri A, Chatel-Chaix L, Schwab Y, Bartenschlager R. 2020. Integrative imaging reveals SARS-CoV-2 induced reshaping of subcellular morphologies. Cell Host & Microbe, 2020 Nov 17:S1931-3128(20)30620-X.
Links:
Team
Get in touch with us




