Tumor diagnosis with different tracers
- 1. [68Ga]Ga and [18F]-PSMA PET-CT studies in patients with primary and recurrent prostate cancer
- 2. [68Ga]Ga-FAPI in patients with esophageal cancer
- 3. FDG and diagnostic MRI in patients with soft tissue sarcomas
- 4. Comparison of [68Ga]Ga-PSMA-11 PET-CT and PET-MRI studies in patients with recurrent prostate cancer
LAFOV PET-CT scanners allow for the first time whole body pharmacokinetic studies with only one measurement. This means that an evaluation of radiotracer kinetics of all organs can be performed simultaneously. Especially in patients with extended metastatic disease, it is for the first time possible to measure simultaneously the tracer uptake in practically all tumor lesions and all organs. This aspect is important particularly for therapy monitoring, drug development and investigation of possible interactions between different organs, known as connectomes.
1. [68Ga]Ga and [18F]-PSMA PET-CT studies in patients with primary and recurrent prostate cancer
Receptor-active peptides enable both the diagnosis and therapy of receptor-active tumors and are used in theragnostic approaches. One of the first examples was [68Ga]Ga-DOTA-TOC, a tracer that binds to somatostatin receptor 2 (SSTR2)-expressing tumors, such as neuroendocrine carcinomas or meningiomas, and is also used for therapy in DOTA-TOC-positive tumors labeled with beta emitters as 90Y or 177Lu. Another example of PRRT are PSMA compounds, which bind to PSMA, a cell surface protein, that is enhanced in prostate carcinoma. The first PSMA used for diagnosis was [68Ga]Ga-PSMA-11, followed by [18F]PSMA-1007. The introduction of these new tracers improved the detection of tumor recurrence and staging of prostate cancer by detecting unknown metastatic lesions with a high contrast to the surrounding tissue. Examples of WB pharmacokinetic studies with both PSMA tracers are presented in Fig. 1a and 1b.

Fig 1a. Combined whole-body dynamic and static PET/CT with low-dose [18F]PSMA-1007 in prostate cancer patients (Sachpekidis C et al. Eur J Nucl Med Mol Imaging 2024; 51:2137-2150)
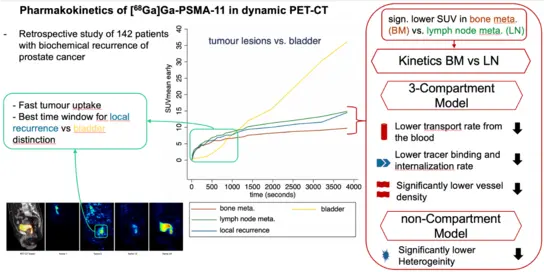
Fig 1b. Pharmacokinetic studies of [68Ga]Ga-PSMA-11 with dynamic PET-CT in patients with prostate cancer (Strauss DS et al. Eur J Nucl Med Mol Imaging 2021; 48:4472-4482)
2. [68Ga]Ga-FAPI in patients with esophageal cancer
Most PET radiopharmaceuticals used in the past targeted more or less different metabolic pathways of the tumor cells. The extraordinary advances in immunotherapy have opened a new era for tracers which target the tumor microenvironment (TME). A novel approach TME is the use of fibroblast activation protein inhibitor (FAPI) imaging in oncological patients, as FAP is known to be overexpressed in the cancer-associated fibroblasts (CAF) of many solid tumors. Several FAPI analogues are available up to now, labeled with 68Ga or 18F, such as [68Ga]Ga-FAPI-46 and [18F]F-FAPI-74. Initial results demonstrate that FAPI may be superior in tumors with low [18F]FDG uptake.
We focus on esophageal cancer and aim to evaluate and compare dynamic PET-CT studies with [68Ga]Ga-FAPI-46 and [18F]FDG Fig. 2a, 2b, 2c).
Cooperation with the Radiation Department of the UKHD (Prof. Dr. Dr. J. Debus) and the Nuclear Department of the University of Mainz (Prof. Dr. M. Schreckenberger).
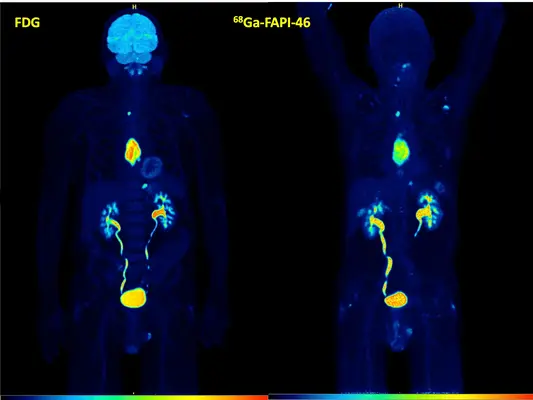
Fig. 2a. FDG vs FAPI in a patient with a primary esophageal cancer. High accumulation of both tracers.
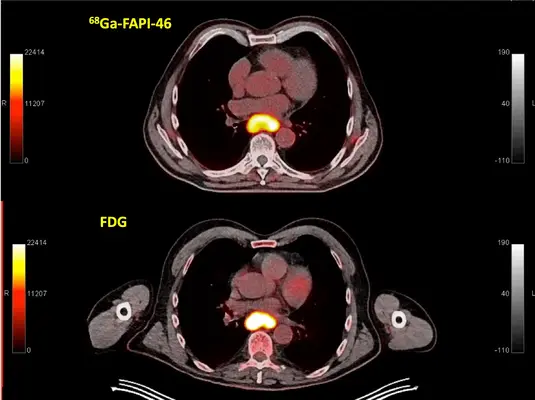
Fig. 2b. FDG vs FAPI of the same patient. Transversal fused PET-CT images in the area of the esophageal cancer both demonstrating a high accumulation.
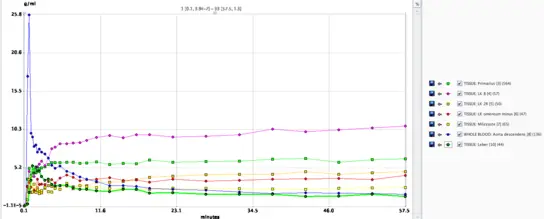
Fig. 2c. FAPI Time activity curves over the primary tumor, lymph node metastases as well as in the descending aorta and in the normal liver parenchyma demonstrating a continuous increase of the malignant lesions over time.
3. FDG and diagnostic MRI in patients with soft tissue sarcomas
The results of whole-body dynamic FDG PET-CT will be compared with those of diffusion-weighted Imaging (DWI) and perfusion-weighted (PWI)-MRI. The comparison of FDG-avid tumor components with diffusion restrictions and pharmacokinetic FDG parameters with PWI-MRI should help in tumor differentiation. Imaging parameters will be correlated to clinicopathological findings in order to explore further imaging characterization. In particular, the identification of aggressive tumor components in the often heterogeneous soft tissue sarcomas is useful before a planned biopsy, as these poorly differentiated areas determine the highest grading and biological behavior of the tumor.
Cooperation with the Radiology of the UKHD (Prof. Dr. U.-H. Kauczor).
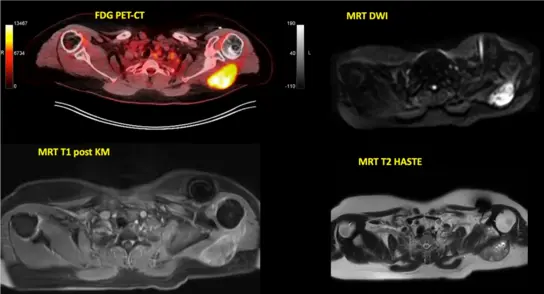
Fig. 3. FDG and diagnostic MRI in a patient with a G3 soft tissue sarcoma located dorsal of the left scapula demonstrating a high FDG accumulation.
4. Comparison of [68Ga]Ga-PSMA-11 PET-CT and PET-MRI studies in patients with recurrent prostate cancer
We compared both hybrid modalities in patients with recurrent prostate cancer and could demonstrate that prostate-bed multiparametric MRI (mpMRI) improves the detection of [68Ga]Ga -PSMA-11 PET-negative local recurrences in a subgroup of prostate recurrencies close to the bladder, which have been superimposed by bladder radioactivity. Hence, the present study demonstrates additional value of hybrid [68Ga]Ga-PSMA-11-PET/MRI by gaining complementary diagnostic information compared to [68Ga]Ga-PSMA-11-PET/CT low-dose in a subgroup of patients with local recurrences very close to the bladder.
Cooperation with the Radiology of the DKFZ (Prof. Dr. Heinz-Peter Schlemmer).
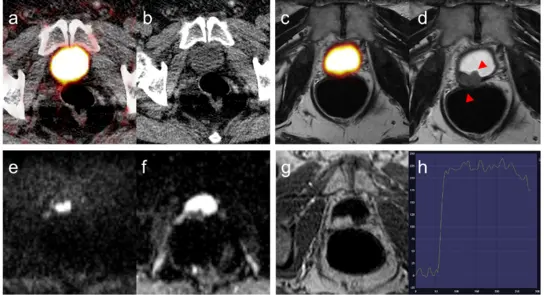
Fig. 4 Example of histologically confirmed local recurrence not delineated in [68Ga]Ga-PSMA-11 PET-CT and PET-MRI due to close proximity to the bladder. PET/CT (a) was negative, low-dose CT was negative (a,b). PET of PET/MRI was negative (c). mpMRI of the prostate bed demonstrates bladder-wall infiltrating local recurrence (red arrow heads) in morphological T2w TSE (d) demonstrating rapid enhancement in T1w-DCE (e,f) accompanied by late wash-out phenomenon. The x-axis in (e) corresponds to time in seconds and the y-axis represents signal intensity in arbitrary units. (Freitag MT et al. Eur J Nucl Med Mol Imaging 2017; 44:776-787)