Applied Functional Genomics
- Functional and Structural Genomics

Prof. Dr. Claudia Scholl
Our laboratory is studying rare, poorly understood tumor diseases with the goal of finding new entry points for therapies through a better understanding of their biology and pathogenesis.
Our Research
Rare cancers and ultra-rare sarcomas pose a major problem for affected patients as they are associated with several challenges. Unlike common cancers, only a few patients are available to conduct randomized clinical trials, discover recurrent cancer driver genes, and study the biology of the disease. This leads to lack of scientific knowledge, misdiagnosis and delays in diagnosis, and deficits in clinical expertise and appropriate therapies, which ultimately results in poorer overall survival when comparing rare to common cancers. The relevance of studying these ill-defined cancers also becomes clear when considering the number of patients affected, which overall are not that rare. 22% of all cancers diagnosed each year in Europe are rare, that is one out of five cancers. In addition, approximately a quarter of all people living with cancer in Europe have a rare cancer, which are 4.3 Million people.
Our strategy to gain insights into the biology of rare cancers is to combine omics analyses of patient samples with the functional characterization of tumor-specific alterations. We have a close cooperation with the prospective precision oncology program MASTER (Molecularly Aided Stratification for Tumor Eradication Research), in which patient tumors, in particular rare cancers, are investigated by whole-genome and RNA sequencing and DNA methylation. Genetic alterations discovered in this program are functionally characterized in our laboratory by using different model systems including cell lines and mouse models. In addition, we uncover secondary gene dependencies by using large-scale CRISPR screening that is followed by their in-depth mechanistic characterization. Through these efforts, we provide new mechanistic insights into critical cellular signaling pathways and help translate genomic information into clinical applications.
Projects
Soft-tissue sarcoma with FUS-TFCP2 or EWSR1-TFCP2 fusions
Rhabdomyosarcoma (RMS) is a soft tissue sarcoma subtype consisting of malignant immature progenitor cells with myogenic differentiation and is thought to originate from skeletal muscle. Our collaborators of the MASTER program (Stefan Fröhling, Christoph Heilig) identified several RMS cases with FUS or EWSR1 fused to the transcription factor TFCP2. These FUS- or EWSR1-TFCP2-positive RMS were recognized in the recently updated WHO classification (2020), but their classification, pathogenesis, and optimal treatment were unclear. In an interdisciplinary effort by our group together with colleagues at DKFZ, NCT Heidelberg, KiTZ, NCT Dresden, and the Institute of Pathology in Münster, we evaluated the clinical, histopathologic, genomic, transcriptomic, and epigenomic features of these patients and studied these tumors' functional and mechanistic underpinnings. Key findings were that TFCP2-rearranged neoplasms should be classified as undifferentiated sarcoma rather than RMS, arise via stepwise sarcomagenesis, and harbor various molecular alterations that represent candidate therapeutic targets, i.e., overexpressed ALK variants, CDKN2A/MTAP co-deletions, and TFCP2 fusion-induced DNA damage repair deficiency. This study illustrates how precision oncology employing comprehensive molecular profiling enables the categorization and biological understanding of rare cancers, which can translate back into new approaches to the clinical management of these often difficult-to-treat entities. (Schöpf, Uhrig, Heilig, Lee et al., Nat Commun 15(1):51, 2024)
Myxoid liposarcoma (MLS)
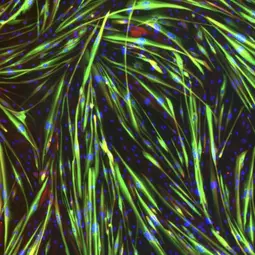
MLS is a malignant tumor of adipocytic origin and is driven by the FUS-DDIT3 fusion gene, which encodes an abnormal transcription factor. By using shRNA screening, we discovered a novel requirement of YAP1 in this cancer type, and demonstrated overactive YAP1 signaling as a unifying feature of MLS development. Mechanistically, FUS-DDIT3 promotes YAP1 expression, nuclear localization, and transcriptional activity and is physically associated with YAP1 in the nucleus of MLS cells. Pharmacological inhibition of YAP1 activity impairs MLS cell growth in vitro and in vivo. Therefore, YAP1 might represent a novel target for therapeutic intervention. This project was carried out together with our long-time cooperation partners Wolfgang Hartmann (Translational Pathology, University Hospital Münster) and Stefan Fröhling (NCT Heidelberg and DKFZ). (Trautmann and Cheng et al., EMBO Molecular Medicine e9889-15, 2019)
One main focus of the lab is the systematic interrogation of essential genes in chordoma. Chordomas are rare but devastating malignant tumors with limited therapy options and incomplete knowledge regarding the pathophysiology of the disease. We are using targeted and large-scale CRISPR screening in human chordoma cells to identify and characterize genes, signaling proteins, and pathways that are essential for the growth of chordomas and may be exploited for the development of novel therapeutic strategies.
In addition, we are developing Designed Ankyrin Repeat Proteins (DARPins) for targeting TBXT in chordoma. The embryonic transcription factor TBXT is highly expressed in nearly all chordomas, but not normal adult tissues, and is required for chordoma cell survival and proliferation. Thus, TBXT represents in principle an attractive therapeutic target, but transcription factors are difficult to inhibit with small molecules. In close collaboration with Prof. Andreas Plückthun (University of Zurich), we are developing TBXT-targeting DARPins, which is a new class of small-protein therapeutics derived from natural ankyrin repeat proteins that recognize and bind their target proteins by mimicking the functional principle of antibodies. (Umbaugh et al., Sci Adv, doi: 10.1126/sciadv.adu2796)

Understanding the molecular and cellular processes involved in lung epithelial regeneration may fuel the development of new therapeutic approaches for lung diseases. We therefore combined new mouse models that allow diphtheria toxin (DTA)-mediated depletion of specific epithelial cell types and GFP-labeling of dividing cells with single-cell transcriptomics to characterize the regeneration of the distal lung. We uncovered new cell types, some of which likely represent epithelial precursors, propose goblet cells as progenitor cells, and provide evidence that adventitial fibroblasts act as supporting cells in epithelial regeneration. We also found that DTA-expressing cells can persist in the lung, express specific inflammatory factors, and resemble a previously undescribed population in the lungs of COVID-19 patients. Our study provides a comprehensive single-cell atlas of the distal lung that characterizes early transcriptional and cellular responses to defined epithelial injury, encompassing proliferation, differentiation, and cell-to-cell interactions. (Martins et al., Nat Commun, 15(1):2246, 2024)
Team
-
Prof. Dr. Claudia Scholl
-

Tara Buschle
-

Dr. Cihan Erkut
-

Usman Shah Gilani
-

Leon-Luca Homagk
-

Sera Kaplan
-

Roman Kurley
-
Leila Martins
-

Denisa-Gabriela Neacsu
-

Stefanie Reinhart
-

Dr. Charles Samuel Umbaugh
-

Jan-Niklas Wittemann
Selected Publications
Charles S. Umbaugh, Marie Groth, Cihan Erkut, Kwang-Seok Lee, Joana Marinho, Simon Linder, Florian Iser, Jonas N. Kapp, Petra Schroeter, Simay Dolaner, Asli Kayserili, Dominic Helm, Martin Schneider, Julia Hartmann, Philipp Walch, Thomas F. E. Barth, Kevin Mellert, Birgit Dreier, Jonas V. Schaefer, Andreas Plückthun, Stefan Fröhling, Claudia Scholl
Leila R. Martins, Lina Sieverling, Michelle Michelhans, Chiara Schiller, Cihan Erkut, Thomas G. P. Grünewald, Sergio Triana, Stefan Fröhling, Lars Velten, Hanno Glimm, Claudia Scholl
Julia Schöpf, Sebastian Uhrig, Christoph E. Heilig, Kwang-Seok Lee, Tatjana Walther, Alexander Carazzato, Anna Maria Dobberkau, Dieter Weichenhan, Christoph Plass, Mark Hartmann, Gaurav D. Diwan, Zunamys I. Carrero, Claudia R. Ball, Tobias Hohl, Thomas Kindler, Patricia Rudolph-Hähnel, Dominic Helm, Martin Schneider, Anna Nilsson, Ingrid Øra, Roland Imle, Ana Banito, Robert B. Russell, Barbara C. Jones, Daniel B. Lipka, Hanno Glimm, Daniel Hübschmann, Wolfgang Hartmann, Stefan Fröhling, Claudia Scholl
Marcel Trautmann, Ya‐Yun Cheng, Patrizia Jensen, Ninel Azoitei, Ines Brunner, Jennifer Hüllein, Mikolaj Slabicki, Ilka Isfort, Magdalene Cyra, Ruth Berthold, Eva Wardelmann, Sebastian Huss, Bianca Altvater, Claudia Rossig, Susanne Hafner, Thomas Simmet, Anders Ståhlberg, Pierre Åman, Thorsten Zenz, Undine Lange, Thomas Kindler, Claudia Scholl, Wolfgang Hartmann, Stefan Fröhling
Get in touch with us