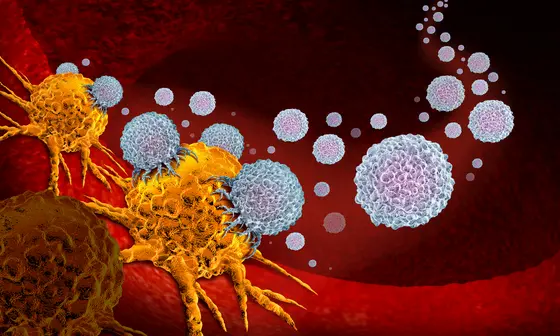
The T cells of the immune system are the main players in the defense against viral infections and tumor cells. On the other hand, they attack the body's own healthy tissue in autoimmune reactions, which can even be fatal. The body must therefore keep a tight control on T cell activity.
A large number of molecules and messenger are involved in the highly complex regulation of T cell activity. Only recently have researchers discovered that another group of immune cells contibutes to the control of T cell activity. Natural killer cells (NK cells) are part of the innate immunity, i.e. the rapid response force that quickly detects and eliminates infected or malignant cells.
“Studies have shown that NK cells can also kill activated T cells and thus limit their proliferation,“ says Michael Platten, Head of Department at the DKFZ and Director of the Neurological University Clinic Mannheim. “However, until now we did not know which feature characterizes T cells as a target for the NK cell.“
When screening activated T cells from healthy donors, Platten's team identified the protein B7H6 as a recognition molecule for NK cell attacks in a new study. Activated T cells from the blood of patients with autoimmune diseases, cancer or viral infections expose large amounts of B7H6 on their surface. Co-culture experiments in the culture dish showed that NK cells recognize the activated T cells by their B7H6 expression. In contrast, T cells whose B7H6 gene was destroyed with the CRISPR-Cas were protected from the lethal attack of the NK cells.
“The elimination of T cells by NK cells is triggered by an intrinsic mechanism of the T cells. The activated T cells temporarily identify themselves as targets for NK-induced cell lysis,“ explains Michael Kilian, first author of the publication, and adds: “This may limit excessive activation and expansion of T cells as a control mechanism to curb destructive immune responses.“
Immune checkpoint inhibitor therapies are neutralized by NK cells
“We now know a number of so-called checkpoint molecules that reduce or enhance the activation of T cells and thus modulate the course of immune reactions. B7H6 can now be classified as a further inhibitory immune checkpoint on T cells,“ explains study leader Platten.
Some widespread cancer therapies with drugs from the checkpoint inhibitor (ICI) group are targeting certain inhibitory checkpoint molecules. They activate the immune system against the tumor by releasing the immune brakes. Could the B7H6-mediated elimination of tumor-reactive T cells possibly counteract the effect of ICI cancer immunotherapy? The researchers tested this using tissue samples from patients with esophageal cancer who had received ICI therapy. Those patients who had not responded to ICI had a higher number of NK cells in the tumor tissue and actually had a shorter progression-free survival time.
Cellular immunotherapy more effective in the absence of NK cells
Cellular immunotherapies are becoming increasingly important in cancer medicine. For example, some forms of blood cancer are now often treated with so-called CAR-T cells, which are equipped with customized receptors against the cancer. However, the success of therapy is often limited as the number of therapeutic cells in the patient's body declines rapidly.
The therapeutic CAR-T cells also carry B7H6 on the cell surface. Could NK cells be responsible for the rapid decline in their numbers after the start of therapy? Experiments with a humanized mouse model suggest this: if NK cells were added during CAR-T cell treatment of leukaemia, the number of therapeutic cells decreased, while the tumour load increased.
“NK control of T cells has the potential to interfere with various forms of cancer immunotherapy. By specifically intervening in this process, it may be possible to modulate T cell immune responses in the future,“ explains Michael Platten, head of the current study. With the help of the CRISPR-Cas gene scissors, the researchers now want to protect CAR-T cells from elimination by NK cells in a clinical trial together with the Department of Haematology and Oncology at Heidelberg University Hospital and thus improve the effectiveness of cellular immunotherapy.
M. Kilian et al.: The immunoglobulin superfamiliy ligand B7H6 subjects T cell responses to NK cell surveillance. Science Immunology 2024, DOI: 10.1126/sciimmunol.adj7970