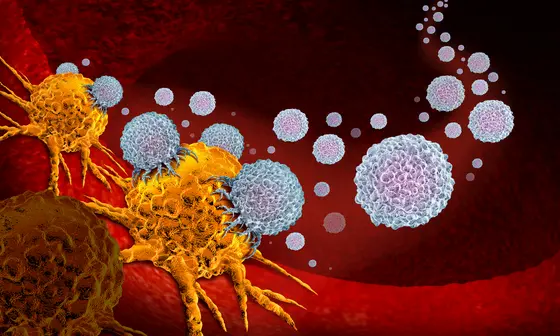
Despite some astonishing successes, immunotherapies fail in many types of cancer. This is particularly tragic in the case of malignant brain tumors, for which there are hardly any effective treatments today. There are several reasons for this failure. Experts believe that the highly immunosuppressive microenvironment of brain tumors is the main cause. It prevents a powerful reaction of the cytotoxic T-cells. This cell type, also known as T-killer cells, is the actual “ executor“ in the defence system's fight against cancer.
T-killer cells migrate into the brain tumors and recognise cancer antigens there - but then quickly lose their ability to function. “Making these paralysed T cells functional again is currently the greatest challenge in the development of immune therapies against brain tumors,“ says Michael Platten, Director of the Department of Neurology at the University Medical Center Mannheim (UMM) and Head of Department at the German Cancer Research Center (DKFZ).
There are indications that, in addition to the T-killer cells, the T-helper cells also play a role in the immune defence against brain tumors. A team led by Michael Platten, Lukas Bunse, DKFZ, UMM and Heidelberg University Hospital (UKHD), and Asaf Madi from Tel Aviv University has now used brain tumor models and patient tissue to investigate under which conditions the helper cells actually contribute to the fight against brain tumors. The researchers' goal is to find approaches for how T killer cells can be trained.
T-helper cells have a peculiarity: they only become active when antigens, for example from viruses or cancer cells, are presented to them on so-called MHCII molecules. The research team has now discovered that in brain tumors, a certain type of immune cells that have migrated from the blood, the myeloid cells, no longer carry these presentation molecules on their surface. This means that myeloid cells are no longer able to activate T-helper cells in the tumor.
Activated helper cells suppress immunosuppressive molecule
If myeloid cells lack the MHCII molecules, killer cells remain inactive, as the researchers have now shown for the first time. The molecular background: Myeloid cells produce large amounts of the immunosuppressive molecule osteopontin, which paralyses the activity of killer cells. However, if T-helper cells are activated by MHCII-present tumor antigens, the osteopontin level drops sharply and T-killer cells regain their functionality.
For the doctors and scientists involved, the study means valuable knowledge that they now want to use to improve immunotherapies against brain tumors. “We now realise that in the development of immunotherapies against brain tumors we must not only rely on cytotoxic killer cells, but absolutely must also take into account T helper cells activated via MHCII,“ says Lukas Bunse, research group leader at the DKFZ and physician at the Department of Neurology at the University Medical Center Mannheim.
“The results also provide clues for the mechanism of action of the vaccine we are developing against brain tumors, which also activates T-helper cells,“ Platten adds. Results of the current study also indicate that treatment with immune checkpoint inhibitors can only boost the immune defence against brain tumors if MHCII-bearing myeloid cells are present. Drug inhibition of osteopontin could also support the immune defence against brain tumors, according to the researchers.
Michael Kilian, Ron Sheinin, Chin Leng Tan, Mirco Friedrich, Christopher Krämer, Ayelet Kaminitz, Khwab Sanghvi, Katharina Lindner, Yu-Chan Chih, Frederik Cichon, Benjamin Richter, Stefanie Jung, Kristine Jähne, Miriam Ratliff, Robert M. Prins, Nima Etminan, Andreas von Deimling, Wolfgang Wick, Asaf Madi, Lukas Bunse, Michael Platten: MHC class II-restricted antigen presentation is required to prevent dysfunction of cytotoxic T cells by blood-borne myeloids in brain tumors
Cancer Cell 2023, DOI: doi.org/10.1016/j.ccell.2022.12.007