The option of chemotherapy can be a difficult one to make when it comes to breast cancer. The treatment can help to reduce tumor size if given before surgery so that less tissue needs to be removed. But it also comes with serious side effects, so that doctors are required to weigh the costs and benefits for each patient. A new study describes tumor-infiltrating lymphocytes (TILs) as an important factor in predicting recovery chances and the usefulness of chemotherapy. Increased TILs indicate that the chemotherapy will be more effective against the tumor.
“Particularly in rapidly growing breast tumors, the presence of immune cells within the tumor tissue is a good indicator of improved response rates. The tumor is then visible to the immune system, “explains Carsten Denkert, of the Institute of Pathology at the Charité, who is one of the breast cancer experts in the DKTK.
Denkert and his colleagues would like to know how reliably the TIL cell content can be used as a biomarker for various types of breast cancer, as well as which immune cell types are the decisive indicators. In this most comprehensive study to date on immune cell infiltrates in breast cancer the research team showed that there can be major differences between tumor subtypes. The scientists analyzed the amount of tumor infiltrating immune cells in 3771 patient tissue samples from six clinical breast cancer studies. All women had received chemotherapy prior to surgery. The study showed that a high TIL content correlates with an improved response to therapy and improved survival rates in patients with so-called triple negative and HER2-positive breast cancer. “In this situation, the chemotherapy and immune system support each other in order to combat the tumor,“ said Denkert.
This is different in the case of the luminal breast cancer subtype (hormone receptor-positive/HER2 negative). Patients with this form of breast cancer typically had lower TIL values and in these tumors TILs did not correlate with higher survival rates. “We believe that there is a different type of immunological infiltrate and a different relation with therapy outcome in this type of breast cancer,“ summarizes Denkert. A closer look revealed that macrophages, which belong to the white blood cells, are indicators of poor prognosis in luminal breast cancer. On the other hand, a high number of antibody-forming B cells, correlates with good survival rates.
“Our results show that the TIL content in certain aggressive forms of breast cancer has a high value in predicting which patients might benefit from chemotherapy,“ emphasized Denkert. For a further improvement of response rates, new immunotherapies are currently being tested which could additionally activate the immune system against the tumor. The DKTK partner site Berlin, in collaboration with the German Breast Group, are conducting biomarker tests in the clinical study GeparNuevo, identify immune cells as as markers for successful immunotherapies with so-called immune checkpoint inhibitors. In the future, TILs could be used as markers to better direct breast cancer treatments for patients.
Original publication:
Denkert et al., Tumor-infiltrating lymphocytes (TILs) and prognosis in different subtypes of breast cancer: a pooled analysis of 3771 patients treated with neoadjuvant therapy. In: Lancet Oncology, Online publication 7th December 2017; DOI: 10.1016/S1470-2045(17)30904-X
An image for the press release can be found at:
Denkert_fig_leftandright.jpg
Image caption:
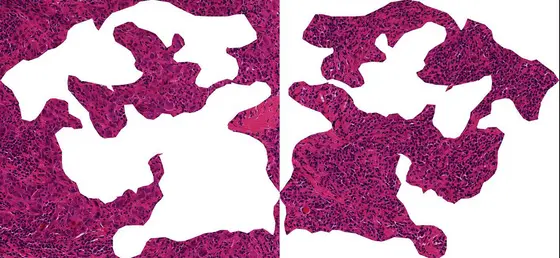
A section through breast cancer tissue: When immune cells (small dark cells) invade the tumor, breast cancer patients have good chances that chemotherapy treatment is effective. The right image shows predominantly tumor cells (round purple cells). In the left image immune cells are infiltrating the tumor.
Note on use of images related to press releases
Use is free of charge. The German Cancer Research Center (Deutsches Krebsforschungszentrum, DKFZ) permits one-time use in the context of reporting about the topic covered in the press release. Images have to be cited as follows: “Source: Hannes Hahne / Susan Klaeger / Bernhard Kuster“.
Distribution of images to third parties is not permitted unless prior consent has been obtained from DKFZ's Press Office (phone: ++49-(0)6221 42 2854, E-mail: presse@dkfz.de). Any commercial use is prohibited.