Medulloblastoma are among the most common solid tumors in children and the most common malignant brain tumor in children. The tumor grows in the cerebellum and can damage vital brain centers as it grows.
Based on tissue characteristics and genetic criteria, medulloblastomas are now divided into different risk groups, which can take a completely different course. While certain subtypes progress aggressively and form metastases, there are other forms that can usually be cured with an intensive combination therapy of surgery, chemotherapy and radiotherapy.
A team of researchers from the Hopp Children's Cancer Center Heidelberg (KiTZ), the German Cancer Research Center (DKFZ) and Heidelberg University Hospital (UKHD) has now used a novel method to investigate what directs certain tumors in a more benign or malignant direction at the cellular level.
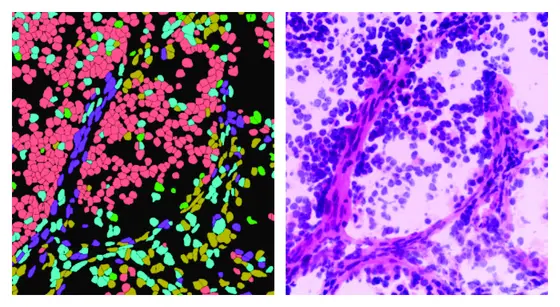
A certain type of medulloblastoma, which is characterized by its good chances of recovery and at the same time by the special structural properties of its tissue, served as a model for them: in so-called medulloblastoma with extensive nodularity (MBEN), small tissue chambers are delimited within the tumor, which are connected in a grape-like manner. The study showed that tumor cells located in these nodules were no longer actively dividing and their genetic program was similar to that of mature brain cells. In the intermediate areas, however, the scientists identified different cell types: In addition to immune and connective tissue cells, there were also significantly more aggressive tumor cells that continued to divide uncontrollably and whose genetic program was more similar to those of fast-growing medulloblastomas and immature nerve cells. In the course of their migration into the nodes, however, the cancer cells matured back into nerve-like cells and no longer divided.
Kristian Pajtler, a pediatric oncologist at KiTZ, DKFZ and UKHD and head of the study, explains the results as follows: “In some childhood tumors, the normal development process is blocked. The cancer cells thus become similar to immature precursor cells, which remain active in division due to a specific genetic program. In MBEN tumors, this apparently only works partially and many of the cells then go through the halfway normal development process of a cerebellar cell and stop dividing. This would also explain the mostly favorable course of this type of tumor.“
For their analyses, the team dissected the tumors of nine young MBEN patients into their individual cellular components and analyzed the genetic program of the individual cells. Using a bioinformatic method, they were then able to reconstruct where exactly these cells were located within the tumor. The method, which was used in collaboration with Karsten Rippe's department at DKFZ, is of particular importance for medulloblastoma research, explains one of the two lead authors of the study, David Ghasemi, physician and scientist at KiTZ, UKHD and DKFZ. “Until now, it has never been possible to develop laboratory models for this type of medulloblastoma. Only with this method was it possible to localize the individual cell types within the tumor and to understand how the various areas within the tumor differ from each other.“
Blocking the maturation process is an important therapeutic tool that is already being researched in order to avert malignant progression in children and steer the cancer cells back in a benign direction. “It is possible that MBEN tumors only need a little push here,“ says Kristian Pajtler. “Because even if most children with an MBEN tumor can be cured by surgery and, if necessary, further therapies, these are very intensive treatments for small children, which are often associated with severe, lifelong side effects.“
Original publication:
Ghasemi D.R., Okonechnikov K. et al. Compartments in medulloblastoma with extensive nodularity are connected through differentiation along the granular precursor lineage. In: Nature Communications (Online Publication 8th of January, DOI: 10.1038/s41467-023-44117-x)
An image for this press release is available for download at:
https://www.kitz-heidelberg.de/fileadmin/media/KiTZ-HD/News/2024/240104-MBEN_MRT.png
Caption:
MRI image: In so-called medulloblastoma with extensive nodularity (MBEN), small tissue chambers are delimited within the tumor and are connected in a grape-like manner.
Note on use of images related to press releases
Use is free of charge. The German Cancer Research Center (Deutsches Krebsforschungszentrum, DKFZ) permits one-time use in the context of reporting about the topic covered in the press release. Images have to be cited as follows: “Source: David Ghasemi /KiTZ“.
Distribution of images to third parties is not permitted unless prior consent has been obtained from DKFZ's Press Office (phone: ++49-(0)6221 42 2854, E-mail: presse@dkfz.de). Any commercial use is prohibited.