Research for a life without cancer
At the DKFZ, we want to ensure that fewer people develop cancer, that cancer can be cured or treated so effectively that those affected can live with the disease and grow old with a good quality of life.
About DKFZ







Latest from DKFZ

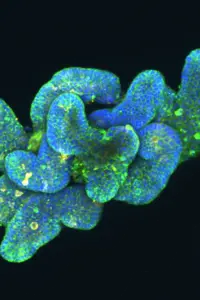
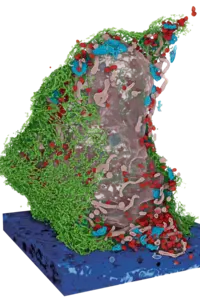
Daniel Kirschenbaum from the German Cancer Research Center (DKFZ) is developing new methods to find out exactly how immune cells are suppressed by malignant brain tumors. He is being supported in this by the EACR-Mark Foundation and the Pezcoller Foundation with the Rising Star Award, which is endowed with 100,000 euros.







Our research opens doors in the fight against cancer


Do you have questions on the topic of cancer?
Let us advise you!
Doctors from the Cancer Information Service answer your questions every day. Find out more now for free!
0800 - 420 30 40 daily from 8 a.m. to 8 p.m.