Research for a life without cancer
At the DKFZ, we want to ensure that fewer people develop cancer, that cancer can be cured or treated so effectively that those affected can live with the disease and grow old with a good quality of life.
About DKFZ







Latest from DKFZ

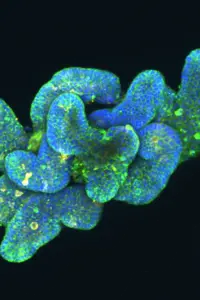
Can the weakened immune systems of older individuals be rejuvenated? Researchers from the German Cancer Research Center (DKFZ), HI-STEM*, and the Broad Institute have demonstrated that this is possible with an innovative approach. In a study now published in Nature, the team showed that mRNA technology can be used to transform the liver in mice into a temporary source of important immune regulatory factors that are naturally lost during aging. This restores the formation of new immune cells, allowing older animals to develop robust immune responses again and fight tumors effectively.







Our research opens doors in the fight against cancer


Do you have questions on the topic of cancer?
Let us advise you!
Doctors from the Cancer Information Service answer your questions every day. Find out more now for free!