Division of Stem Cells and Cancer
Prof. Dr. Andreas Trumpp
Stem cells are essential for maintaining
and repairing regenerative tissues. However,
genetic alterations of stem cells can
lead to the generation of “cancer stem
cells” (CSCs) that drive tumorigenesis and
metastasis. Starting with mouse models,
we extend our work to the analysis of primary
patient samples (blood, bone marrow,
tumor/metastasis samples) and link the
results to clinical parameters with the goal
to develop innovative strategies to detect
and target cancer and metastatic stem
cells and break therapy resistance (see also:
www.hi-stem.de).
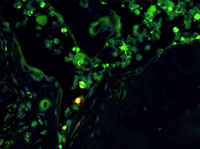
We are interested to unravel the molecular
and cellular basis of hematopoietic stem
cell (HSC) and embryonic stem cell (ESC)
self-renewal. We have previously shown
that the most potent HSCs are in a state of
deep dormancy. In response to infections
or chemotherapy mediated cell loss, dormant
HSCs become activated and organize
the repair of the system (Wilson, Cell 2008;
Essers, Nature 2009). Using genome-wide
transcriptomics, proteomics and methylome
analysis, we have established the
molecular landscape of HSCs and progenitors
to understand the molecular basis
of self-renewal and multipotency, as well
as the interactions between stem cells
and their niche (1). We then showed that
the oncogene MYC controls dormancy of
pluripotent cells in the embryo and HSCs
in the adult organism. Thus, MYC is the
key regulator controlling entry and exit
from dormancy of normal stem cells and
potentially in cancer and metastasis stem
cells (2). In our MDS and AML program we
study signaling networks and the role of
the microenvironment for disease progression
and therapy resistance (Medyouf, Cell
Stem Cell 2014). In solid tumors, we have
identified circulating “metastasis initiating
cells” (MICs) directly from the peripheral
blood of breast cancer patients, which
are able to initiate new bone and lung
metastasis. Their cell surface receptors
CD44+MET+CD47+ offer now novel possibilities for the design of better diagnostic
and therapeutic tools for breast cancer (3).
In pancreatic cancer we have identified
novel tumor subclasses and developed
biomarkers to allow the stratification of
patients. One subclass shows a widespread
resistance to current therapies. This is mediated
by CYP3A5, which initiates an enzymatic
cascade to metabolize and inactivate
the drugs. Blockade of CYP3A5 breaks resistance and sensitizes the tumors to
several drugs in preclinical settings (4). We
are now developing CYP3A5 inhibitors for
combination therapies to target pancreatic
cancers.
Future Outlook:
We functionally characterize both normal
and malignant stem cells by using in vitro
and in vivo approaches. We then use stateof-
the-art methods to uncover the mechanisms
that control and drive normal and
uncontrolled self-renewal as well as therapy
resistance. From model systems, we
typically extend our work to the analysis of
primary patient derived samples and link
the results to clinical parameters with the
goal to develop innovative strategies to detect
and target cancer and metastatic stem
cells and break therapy resistance.
In addition to his role as Head of the Division of Stem Cells and Cancer, Prof. Trumpp is also Managing Director of the Heidelberg Institute for Stem Cell Technology and Experimental Medicine, located within the main building of the DKFZ.
Click here for more details.